INFLAMMATION - Can't live with it & can't live without it
Inflammation is a double-edged sword: it’s essential for healing and defending our body against pathogens, but chronic inflammation can lead to various health issues and diseases.
COMPLETE GUIDE to Understanding Inflammation in the Body

WHAT IS INFLAMMATION?
Inflammation is a defensive reaction of the immune system, naturally activated to protect the body against harmful stimuli. learn more
What is Inflammation caused by?
- Exposure to toxins (pollution, chemicals)
- Infections or injury
- Obesity (high BMI body mass index)
- Lack of physical activity
- Poor sleep
- Chronic stress
- Alcohol & Smoking
The role of inflammation in health and disease is crucial. Acute inflammation plays a vital role in fighting infections, healing injuries, and restoring tissue balance. However, chronic inflammation can have detrimental consequences, as it may lead to the damage of healthy tissues and the development of chronic diseases.
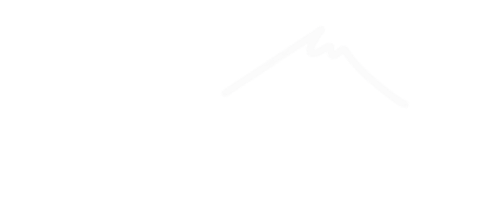
TYPES OF INFLAMMATION?
The Simple Explanation
- ACUTE INFLAMMATION
- SUB-ACUTE INFLAMMATION
- CHRONIC INFLAMMATION
Acute inflammation is the body’s natural response to injury or harmful stimuli, like infections, burns, or cuts. It’s a short-term process that aims to protect and heal the body. Imagine you accidentally cut your finger while slicing vegetables. The area becomes red, swollen, warm, and painful. This is acute inflammation in action. It’s like the body’s alarm system, bringing white blood cells to the injured spot to fight off any germs and start the healing process. Once the threat is dealt with and healing starts, the inflammation gradually subsides.
Acute inflammation is the body’s quick and temporary response to fix problems and get things back to normal.
Sub-acute inflammation is a stage between acute (short-term) and chronic (long-term) inflammation. It lasts a bit longer than acute inflammation but not as long as chronic inflammation. Think of it as a middle ground. For example, if you have a mild infection that doesn’t go away quickly, your body might keep sending white blood cells for a bit longer. This is sub-acute inflammation. It’s not a full-blown ongoing issue like chronic inflammation, but it’s more than the quick response of acute inflammation. The body is still working to heal, but it’s taking a little longer.
Sub-acute inflammation can happen when the body needs extra time to completely clear out the problem, like when dealing with infections that are a bit tougher to handle.
Chronic inflammation is like a persistent, long-term alarm in your body that doesn’t turn off properly. It happens when your immune system keeps trying to fight something even when it’s not needed. Imagine a situation where your body thinks there’s a problem, like a small splinter that’s hard to remove. Instead of stopping the alarm once the splinter’s out, the alarm keeps ringing. Over time, this can cause damage to your body’s tissues and organs. For instance, chronic inflammation might play a role in conditions like arthritis, where joints become swollen and painful for a long time.
Chronic inflammation is when your body’s defence system doesn’t know when to stop, and it can lead to bigger health issues.
An In-depth Look at Inflammation in the Body
Now let’s get into the detailed explanation about the triggers & causes of acute and chronic inflammation

CAUSES OF INFLAMMATION IN THE BODY
Understanding Acute Inflammation: Triggers and Causes Explained
Acute inflammation is often triggered by infectious agents, including bacteria, viruses, fungi, and parasites. When these pathogens enter the body, the immune system recognises them as foreign invaders and mounts an inflammatory response to eliminate them. The process starts with immune cells detecting the presence of the pathogens or their components, such as pathogen-associated molecular patterns (PAMPs).
This recognition triggers the release of inflammatory cytokines and chemokines, which recruit immune cells to the site of infection. Neutrophils, monocytes, and macrophages are key immune cells that play a crucial role in combating the infection through phagocytosis, where they engulf and destroy the invading pathogens. This acute inflammatory response creates an environment that is less favorable for the pathogen’s survival and helps contain and clear the infection.
Physical injuries, such as cuts, burns, sprains, fractures, and abrasions, cause immediate tissue damage and expose the underlying tissues to the external environment. Injured tissues release molecules known as damage-associated molecular patterns (DAMPs), which are recognized by the immune system as signals of cellular damage. DAMPs activate the inflammatory response by recruiting immune cells to the injury site.
Neutrophils are the first responders and arrive within hours of the injury to remove debris and prevent infection. Macrophages follow, performing phagocytosis and secreting growth factors that stimulate tissue repair. The acute inflammatory response in the case of injuries is essential for initiating the healing process, including tissue regeneration and forming new blood vessels.
Acute inflammation triggered by allergens is characteristic of allergic reactions. Allergens are typically harmless substances that the immune system of allergic individuals perceives as threats. Common allergens include pollen, dust mites, pet dander, certain foods (e.g., nuts, shellfish), and insect venom. When an allergic individual comes into contact with an allergen, their immune system produces specific immunoglobulin E (IgE) antibodies against it.
Upon subsequent exposure to the same allergen, the IgE antibodies recognize it and trigger the release of histamine and other inflammatory mediators from mast cells and basophils. This leads to the dilation of blood vessels, increased vascular permeability, and the characteristic symptoms of acute inflammation, such as itching, redness, swelling, and mucus production.
Exposure to irritating substances, such as chemicals, smoke, air pollution, or harsh cleaning agents, can induce acute inflammation in the affected tissues. These irritants can directly damage cells or cause irritation and inflammation by interacting with the body’s tissues.
For example, exposure to airborne pollutants in the respiratory system can irritate the airways, leading to an acute inflammatory response with symptoms like coughing, wheezing, and shortness of breath. In the skin, contact with irritants can cause dermatitis, characterised by redness, itching, and swelling.
In some autoimmune diseases, the immune system mistakenly identifies the body’s tissues as foreign and mounts an inflammatory response against them. The exact triggers for autoimmune reactions are not always well understood, but they often involve a combination of genetic predisposition and environmental factors. Autoimmune diseases can affect various organs and tissues, leading to localised or systemic acute inflammation.
For instance, in rheumatoid arthritis, the immune system attacks the synovium (the lining of joints), causing inflammation, pain, and joint damage. Inflammatory bowel diseases like Crohn’s disease and ulcerative colitis involve chronic inflammation of the gastrointestinal tract due to autoimmune reactions.
Chronic inflammation (unlike acute inflammation) is not a healthy response and can lead to tissue damage and various chronic diseases. Its a prolonged and persistent inflammatory response that can last for months or years. The triggers and causes for chronic inflammation are more complex and may include…
Understanding Chronic Inflammation: Triggers and Causes Explained
Chronic inflammation can happen if the immune system doesn’t fully get rid of infections, or if infections aren’t treated right. Some germs can hide from the immune system, causing long-term inflammation. Diseases like tuberculosis and hepatitis C can keep the body in this inflamed state. Over time, this can damage body tissues and may lead to serious health issues.
Autoimmune disorders are conditions in which the immune system mistakenly attacks the body’s own tissues, leading to chronic inflammation in specific organs or tissues. In autoimmune diseases like rheumatoid arthritis, the immune system targets the synovial membrane (lining of joints) and other connective tissues, causing persistent inflammation and joint damage. In systemic autoimmune diseases like systemic lupus erythematosus (lupus), multiple organs can be affected, leading to widespread chronic inflammation. Inflammatory bowel diseases (IBD), such as Crohn’s disease and ulcerative colitis, involve chronic inflammation of the gastrointestinal tract due to autoimmune reactions.
Certain lifestyle choices can contribute to chronic low-grade inflammation, which is a milder, persistent form of inflammation that doesn’t produce obvious symptoms but can still lead to health issues over time. Poor dietary habits, such as consuming a diet high in processed foods, unhealthy fats, refined sugars, and low in fruits and vegetables, can promote inflammation. Excessive alcohol consumption and smoking can also exacerbate chronic inflammation. Sedentary behaviour and lack of regular physical activity have been associated with increased levels of inflammation markers in the body.
Obesity is a significant risk factor for chronic inflammation. Adipose tissue, or fat cells, can produce and release pro-inflammatory molecules called adipokines. As body fat increases, the adipose tissue becomes more metabolically active and releases higher levels of these inflammatory substances, contributing to a state of chronic inflammation. This chronic low-grade inflammation in obesity has been linked to insulin resistance, cardiovascular disease, and other obesity-related health conditions
Being exposed to pollution and toxins over a long time can cause lasting inflammation in the body. This is due to the immune system being persistently activated. Also, chronic stress triggers our ‘fight or flight’ response, which, if activated too often, can lead to an imbalance in the immune system and keep the body inflamed. This ongoing inflammation can make stress-related health problems even worse.
As we age, chronic inflammation becomes more common. This is due to changes in the immune system and the buildup of damage to our cells over time. Such inflammation is linked to diseases common in older adults, like heart and brain disorders, and diabetes. That’s why adopting an anti-inflammatory lifestyle early on is key to better long-term health.
Epigenetic changes are modifications in the structure of our DNA and proteins. These changes can influence how genes are activated (turned on) or silenced (turned off) in response to various signals and environmental factors.
In the context of chronic inflammation, epigenetic changes play a significant role. When inflammation becomes chronic, it can lead to a state where specific genes responsible for controlling the immune response and inflammation are continuously activated.
Over time, diet, stress, exposure to pollutants, and other lifestyle elements can cause epigenetic modifications. As a result, genes that promote inflammation might be switched on more frequently, while genes that would usually suppress inflammation might be switched off. This creates a self-perpetuating cycle of inflammation, where the body’s immune system stays activated even when there is no actual threat or injury to fight off.
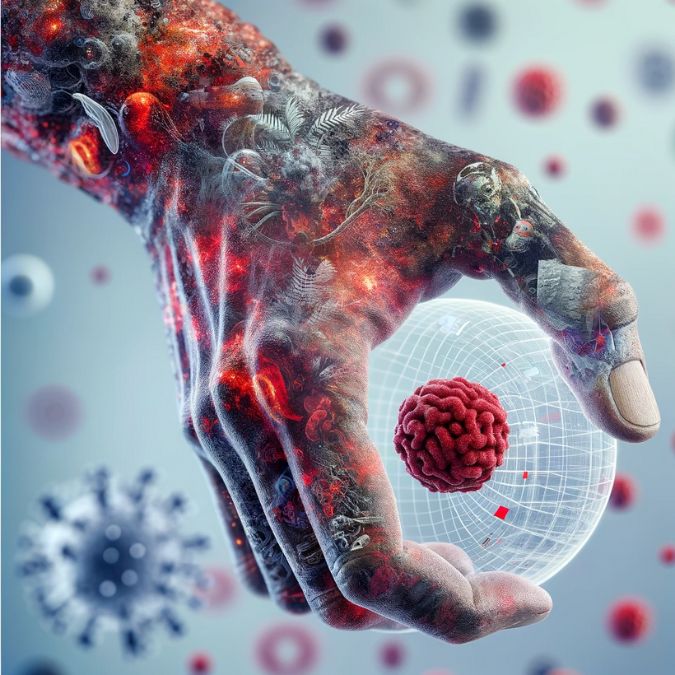
Now that we understand the causes and triggers, let’s examine the inflammation process. What’s going on in the body? To make it easier to understand, let’s use the fire alarm analogy.
UNDERSTANDING THE INFLAMMATION PROCESS
The Inflammation Response: A Fire Alarm in Your Body
Imagine a fire alarm going off when there’s danger. First, something triggers the alarm, like an injury or a germ. This is the start of inflammation. Then, our body’s “firefighters,” called immune cells, rush to the scene to fight off the danger. This can cause redness, swelling, and heat as they work. As the danger is dealt with, the immune cells calm down, and the alarm stops.
- RECOGNITION
- ACTIVATION
- VASODILATION
- RECRUITMENT
- REPAIR
- RETURN
Recognition Phase: In this initial phase of inflammation, the immune system’s watchful cells, such as macrophages and dendritic cells, act as vigilant sentinels. They scan the body, searching for any signs of trouble like harmful microbes, injuries, or damaged cells. When these guardians detect something amiss, they sound the alarm, initiating the body’s defence response.
Activation Phase: Once the alarm is raised, immune cells release chemical messengers like cytokines and prostaglandins. These messengers serve as urgent calls for reinforcements. Think of them as the body’s way of saying, “Help! There’s a problem here!” These signals kickstart the inflammatory response, alerting nearby cells and blood vessels to prepare for action.
Vasodilation Phase: During this phase, blood vessels near the affected area widen or dilate. This dilation increases blood flow to the site of inflammation, resulting in visible signs such as redness and warmth. It also allows immune cells, antibodies, and essential nutrients to quickly move from the bloodstream into the inflamed tissues, helping the body fight off invaders. Additionally, increased permeability of blood vessels allows fluid to accumulate, leading to swelling, which can be protective.
Recruitment Phase: In response to the distress signals, immune cells like neutrophils and macrophages are summoned to the site of inflammation. These cells are the first responders, working to neutralize pathogens (like bacteria or viruses) and clean up damaged tissue. They play a crucial role in the body’s defence against infections and injury.
Repair Tissue Phase: Inflammation isn’t just about defence; it also promotes healing. This phase stimulates the production of new cells and tissues necessary for repairing the damage caused by infection or injury. It’s like sending in construction crews to rebuild and restore the affected area.
Return Phase: After the job is done, a healthy body naturally returns to its balanced state, known as homeostasis. In this phase, the inflammation subsides, and the body’s systems resume their usual functions. However, in cases of chronic inflammation, this return to balance is disrupted, potentially leading to ongoing health issues and complications. Maintaining a healthy anti-inflammatory lifestyle can help support a smooth return to homeostasis.

In chronic inflammation, the alarm keeps ringing even when there’s no more danger. This ongoing alarm can damage healthy parts of the body, leading to severe problems over time, even altering our DNA!
Did you know? Chronic Inflammation can alter your DNA!
Epigenetic changes are adjustments to our DNA that regulate gene activity without altering the DNA sequence itself. They act as dimmers, adjusting the expression of various genes, including those involved in inflammation. Chronic inflammation can disrupt these settings, leaving the inflammatory response permanently on. This disruption can be caused by factors like diet, stress, and toxins, leading to continuous false alarms in the body’s defences system.
Prolonged inflammation may eventually lead to damage in body tissues, disrupt normal organ function, and increase the risk of diseases such as heart conditions, diabetes, cancers, and brain-related disorders. Controlling chronic inflammation means tackling these epigenetic disturbances by leading a healthy lifestyle, treating persistent conditions, and possibly adjusting epigenetic markers through medical interventions.

DIAGNOSTIC TECHNIQUES FOR INFLAMMATION
Self-assessment involves tuning into your body’s signals to detect signs of inflammation. While not a substitute for professional medical evaluation, it can provide early awareness. If you consistently experience pain, swelling, warmth, or redness in a particular area, it might indicate inflammation. Keeping a record of symptoms and their duration can assist your doctor in making an accurate diagnosis. However, other health conditions can mimic inflammation’s symptoms, so seeking medical advice is crucial for proper diagnosis and treatment.
Blood tests are valuable tools in diagnosing inflammation. They measure specific substances in the blood that increase when inflammation is present. C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are commonly measured markers. Elevated levels of these markers suggest inflammation. These tests provide insights into the severity of inflammation and help doctors monitor the effectiveness of treatments. While blood tests are sensitive to inflammation, they don’t always pinpoint the exact cause. Further testing and evaluation are often needed to determine the underlying issue.
Imaging techniques like X-rays, CT scans, and MRI scans are crucial in visualising internal structures to identify inflammation-related changes. X-rays are beneficial for detecting inflammation in bones. CT scans provide detailed cross-sectional images, aiding in identifying inflammation in soft tissues and organs. MRI scans offer detailed views of soft tissues, helping diagnose inflammation in joints, muscles, and the nervous system. Imaging can reveal swelling, damage, and changes in structure caused by inflammation. However, imaging alone might not determine the cause of inflammation, requiring correlation with other clinical information.
Biopsies involve removing a small tissue sample from an area suspected of inflammation for microscopic examination. This direct assessment provides valuable information about the type and severity of inflammation, aiding in diagnosis and treatment planning. Biopsies are especially valuable in chronic inflammation cases where other diagnostic methods might not provide a clear answer. They also help differentiate between different conditions that share similar symptoms. However, biopsies are invasive and carry some risks, such as infection or bleeding. The decision to perform a biopsy is usually based on the clinical situation and its potential benefits in guiding treatment decisions.
How to Reduce Inflammation in the Body!
MANAGING & TREATING INFLAMMATION
Dietary Adjustments: Anti-inflammatory diets rich in fruits, vegetables, lean proteins, and whole grains can reduce inflammation markers. Foods high in omega-3 fatty acids, like salmon and flaxseeds, are particularly effective. Avoiding processed foods, excessive sugar, and saturated fats is also crucial. This approach is not a quick fix but a long-term strategy for overall health.
Regular Exercise: Engaging in regular physical activity helps to lower the risk of chronic inflammation. This doesn’t mean you need to run marathons; even moderate activities like walking, swimming, or cycling can be beneficial. The key is consistency and finding an activity that you enjoy and can stick with.
Stress Reduction: Chronic stress is a known contributor to inflammation. Techniques such as meditation, deep-breathing exercises, and yoga can help manage stress levels. Seeking out hobbies or activities that bring relaxation can also help in reducing stress-induced inflammation.
Medications and Supplements: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) can provide immediate relief from acute inflammation. But they are a dangerous long-term treatment option making them unsuitable for chronic inflammation. Natural Supplements such as turmeric, ginger, and moringa oil have shown potential benefits, but they’re not a silver inflammation killing bullet.
Medical Interventions: When lifestyle changes are not enough, or if an underlying condition is causing inflammation, medical treatment may be necessary. This could include prescription medications like corticosteroids or disease-modifying antirheumatic drugs (DMARDs) for autoimmune diseases. Physical therapy can also be beneficial for inflammation caused by injuries or chronic conditions.
Anti-Inflammatory Lifestyle Changes: (Feel Better Faster in 3 weeks or less):
FBF3 is a comprehensive framework designed to ease inflammation and stress through five key practices: mindful eating for weight management, regular physical activity for robust fitness, stretching to improve flexibility, breathwork techniques for calming, and mindfulness practices for mental equilibrium. These 5 elements collectively nurture and support health holistically.
Hydration: Adequate water intake can help flush out toxins that may contribute to inflammation.
Healthy Sleep Habits: Getting enough sleep is essential for the body’s healing processes, including reducing inflammation.
Avoiding Irritants: Reducing exposure to environmental irritants, like pollution and second-hand smoke, can prevent unnecessary immune responses.
Proper Body Weight: Maintaining a healthy weight can decrease the strain on the body and lower levels of inflammatory substances produced by body fat.
Professional Guidance: Regular check-ups and discussions with healthcare professionals can ensure you’re on the right track and adjust treatments as needed.
*Each of these areas plays a role in a holistic approach to managing inflammation and can be tailored to fit individual health needs and lifestyles.
BUY Anti-Inflammatory Supplements & Anti-Inflammatory Foods

PREVENTION OF INFLAMMATION
Anti-Inflammatory Lifestyle Changes
Embracing an anti-inflammatory lifestyle is like this five-pointed star, each point symbolizes a holistic health practice. Mindful eating for weight control, physical activity for fitness, stretching for flexibility, breathwork for stress relief, and mindfulness for mental balance. Each aspect is integral, working in harmony to support and enhance overall health. learn more

WHEN TO SPEAK TO YOUR DOCTOR ABOUT INFLAMMATION?
You should consult your doctor for chronic inflammation if you notice persistent symptoms such as ongoing pain, fatigue, insomnia, or issues like weight gain and digestive problems that don’t resolve over time. For acute inflammation, such as from an injury or infection, see a doctor if you experience severe swelling, redness, pain that intensifies or doesn’t improve within a few days, or if you have a fever. It’s crucial to get medical advice to manage inflammation properly and address any underlying conditions that may contribute to it.
In Conclusion
Inflammation is a critical process that serves as the body’s defense mechanism against harm and aids in the healing process. While acute inflammation is a necessary and beneficial response, chronic inflammation can lead to various health issues.
Understanding the causes, types, processes, and management of inflammation is essential for maintaining overall health and preventing the development of chronic diseases. By adopting a healthy lifestyle and seeking appropriate medical attention when needed, individuals can promote a balanced inflammatory response and support their well-being.
Compleate Guide to Understanding Inflammation in the Body – Further Reading